Your doctor says that you should undergo a cataract surgery…
What should you expect in the days following the operation? What precautions should be taken? Dr. Li Yim, an ophthalmologist at the Clinique Bon Pasteur, has accepted to answer all our questions.
What to expect in the days following the surgery?
Although a cataract surgery is generally painless, discomfort or pain may occur during the hours following the operation. However, they should pass quite quickly. Bleeding in the white part of the eye is also often observed, and it usually lasts 5 to 7 days. Vision will be blurred after the procedure, but will gradually return to normal within 2 hours, after a local anaesthesia.
It is also normal for the pupil to remain dilated for 12 to 24 hours. Finally, an increased sensitivity to light, or the impression of ‘seeing flies’ or floating bodies, may happen in some cases. Everything should settle within four weeks.
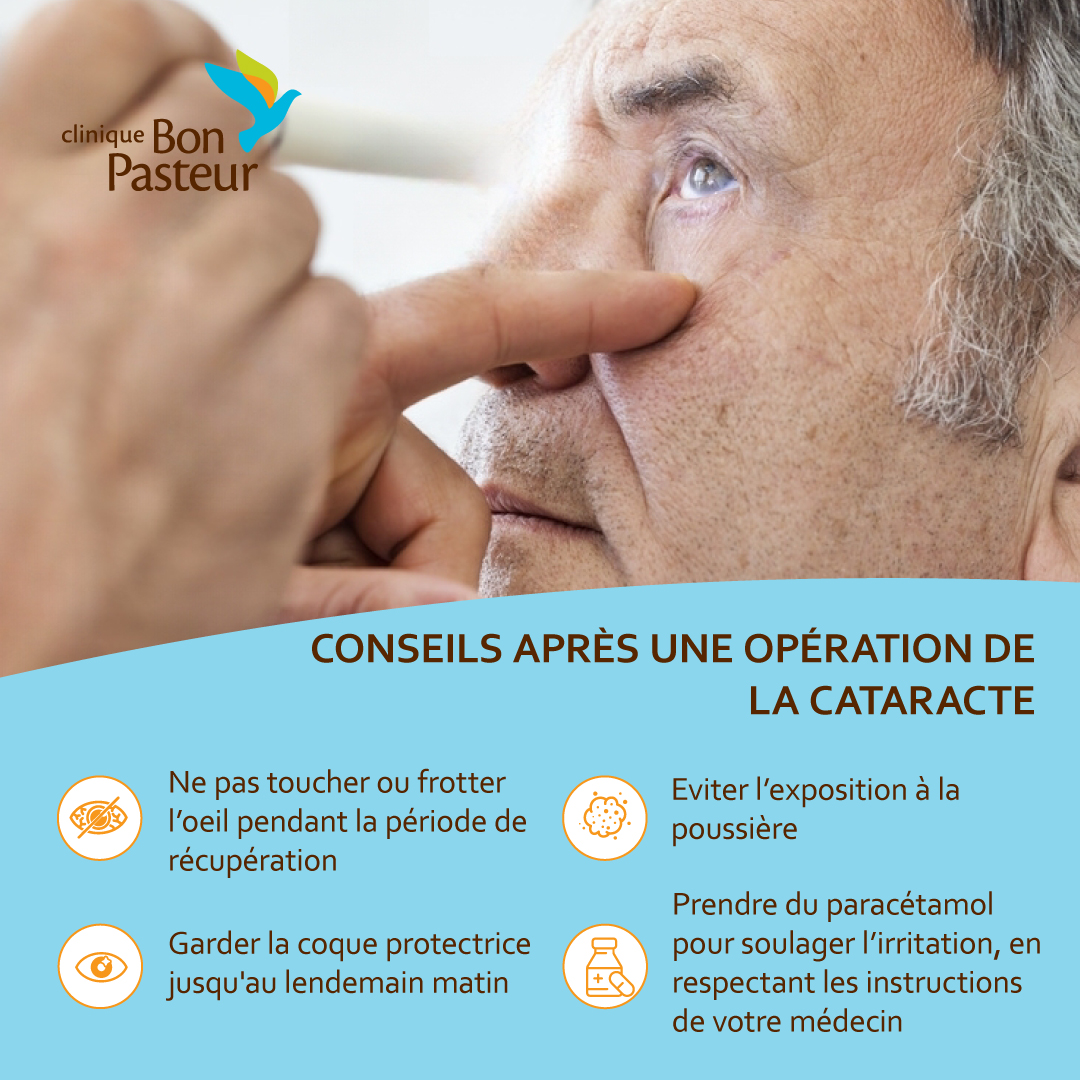
What precautions should be taken in the evening after the procedure?
It is normal to feel a slight irritation in the eye with each blink. You can therefore take a little paracetamol to ease the discomfort. Apart from this, the eye shield must be kept on until morning. On the first night, no eye drops are applied so as to let the eye rest.
And the next day?
You can remove the eye shield as soon as you wake up. Make sure not to rub your eye! You can nevertheless clean your eye using a cotton pad soaked in previously boiled, warm water, but without exerting any pressure!
You can start your eye drop treatment – Pred Forte and Exocin – ahead of the post-operative visit. Make sure to shake the bottles well before use, then squeeze one drop from each bottle into each eye, waiting 5 minutes in between; you should repeat the process every 4 hours, during waking hours. The duration of treatment depends on the prescribed medication: it is advisable, for example, to stop Exocin after 1 week, but to continue Pred Forte for a whole month.
Are there any special precautions to take?
Of course. During the first week, avoid rubbing your eyes. You should also be careful not to let dust, shampoo or soap into your eye. Moreover, avoid wearing makeup or applying cream in the eye area for two weeks.
You can, however, resume your activities: there are no dietary restrictions, and you can even watch TV and read your book the day after the operation! Make sure to wash your hands regularly throughout the day.
Listen to your body: after your postoperative visit, if you experience pain, more redness, a decrease in your vision, a feeling of veil on the eye, or if you see flashes of light or floating bodies, do not hesitate to contact your ophthalmologist.
For more information, call us on 401 95 00 or send us a WhatsApp message on 5 835 38 86.